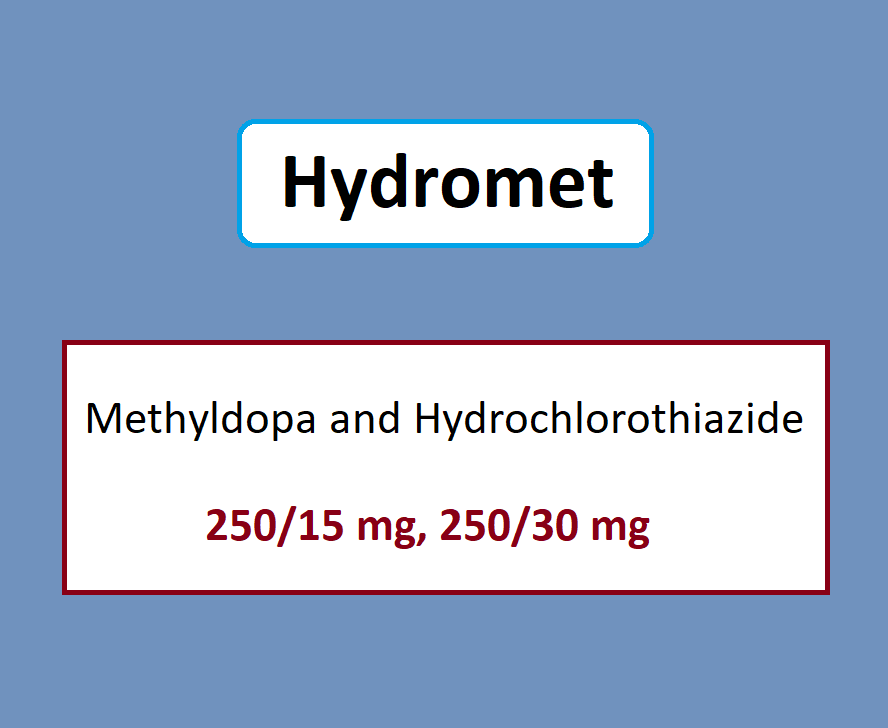
Hydromet is a combination of two drugs, methyldopa, and hydrochlorothiazide. Methyldopa is a centrally acting drug that reduces the sympathetic outflow to the heart, kidneys, and blood vessels. Hydrochlorothiazide is a diuretic that reduces intravascular volume.
Hydromet (Methyldopa and hydrochlorothiazide) Uses:
-
Hypertension:
- Used in management of hypertension
Methyldopa and hydrochlorothiazide Dose in Adults:
Methyldopa and hydrochlorothiazide (Hydromet) Dose in the treatment of Hypertension: Oral:
Note: Dose is individualized.
-
Replacement therapy:
- Initial:
- Methyldopa 250 mg per hydrochlorothiazide 15 mg 2 to 3 thrice time in a day or methyldopa 250 mg per hydrochlorothiazide 25 mg twice in a day or methyldopa 500 mg per hydrochlorothiazide 30 mg once in a day or methyldopa 500 mg/hydrochlorothiazide 50 mg once in a day.
- Maximum each day dose, based on the hydrochlorothiazide content:
- Oral: 50 mg per day.
- Initial:
Use in Children:
Not indicated.
Pregnancy Risk Factor: C
- This combination has not been used in animal reproduction studies.
- See Methyldopa and hydrochlorothiazide
Use of hydrochlorothiazide and methyldopa during breastfeeding
- Breast milk contains hydrochlorothiazide and methyldopa.
- The manufacturer warns that there are serious adverse reactions for nursing babies and recommends that a decision is made about whether to stop nursing or stop using the drug.
- This should be done taking into consideration the importance of mother's treatment.
Methyldopa and hydrochlorothiazide (Hydromet) Dose in Kidney Disease:
- There are no dosage adjustments provided in the manufacturer's labeling (use is contraindicated with anuria).
- The following adjustments have been recommended for hydrochlorothiazide:
- CrCl ≥10 mL/minute:
- No dosage adjustment is necessary.
- Usually ineffective with CrCl <30 mL/minute unless in combination with a loop diuretic.
- CrCl <10 mL/minute:
- Use not recommended.
- CrCl ≥10 mL/minute:
Dose in Liver disease:
There are no dosage adjustments provided in the manufacturer's labeling; use is contraindicated in patients with active hepatic disease.
Methyldopa and hydrochlorothiazide (Hydromet) Side effects:
See individual agents (Methyldopa and hydrochlorothiazide)
Contraindications to Methyldopa and hydrochlorothiazide (Hydromet):
- Hypersensitivity to hydrochlorothiazide or sulfonamide derived drugs, methyldopa or any component in the formulation
- Active cirrhosis (active cirrhosis), acute hepatitis
- Hepatic disorders were previously linked to the use of methyldopa
- Use of MAO inhibitors concurrently
- Anuria
Notification:
- FDA approved product labeling that states this medication is contraindicated when used with other sulfonamide-containing drug classes has been challenged.
- There is not much evidence of cross-reactivity between thiazide-related diuretics and allergens.
- Cross-sensitivity is possible due to similarities in chemical structure and/or pharmaceutical actions.
- However, this cannot be excluded with absolute certainty.
Warnings and precautions
-
Electrolyte disturbances:
- Hydrochlorothiazide can cause hypokalemia, hypochloremic acidkalosis, hypomagnesemia and hyponatremia.
-
Gout
- Hydrochlorothiazide can trigger gout in certain patients who have a history of gout or are at risk for chronic renal failure.
- Doses of 25 mg and more can increase the risk.
-
Hematologic effects
- With methyldopa, rare cases of reversible Granulocytopenia or Thrombcytopenia have been reported.
- Hemolytic anemia is rare; positive Coombs test results in 10% to 20% of patients often occur between 6 and 12 month of treatment; periodically perform CBC.
- If Coombs' positive hemolyticanemia occurs during therapy, stop using it and do not restart.
- Coombs may not return to normal for several weeks or months after discontinuation.
-
Hepatic effects
- Patients with liver disease or dysfunction may experience liver problems, including fatal hepatic necrosis.
- Monitor your liver function every 6-12 weeks or whenever unexplained symptoms occur.
- If fever, abnormal liver function tests or jaundice are present, discontinue therapy.
-
Hypersensitivity reactions
- Hydrochlorothiazide may cause hypersensitivity reactions.
- Patients with a history bronchial or allergy disorder are at greater risk.
-
Neuromuscular effects:
- Rarely have patients with severe bilateral cerebrovascular diseases displayed involuntary choreoathetotic movements using methyldopa.
- If any of these symptoms develop, it is important to stop treatment.
-
Ocular effects
- Patients with acute visual acuity and ocular pain may experience hydrochlorothiazide-induced transient myopia or acute angle-closure vision loss.
- If intraocular pressure is not controlled, additional treatments may be required.
- Risk factors may include penicillin allergy or history of sulfonamide allergy.
-
Photosensitivity
- Hydrochlorothiazide may cause photosensitization.
-
Sedation
- Sedation is usually temporary and may occur during initiation or when the dose of methyldopa increases.
-
Allergy to sulfonamide ("sulfa")
- Potential for cross-reactivity among members of a particular class (eg two antibiotic sulfonamides).
- Cross-reactivity concerns have been raised for all compounds with the sulfonamide structural.
- FDA approved product labeling of many medications that contain a sulfonamide chemical class.
- This includes a wide contraindication for patients who have had an allergic reaction to sulfonamides in the past.
- Nonantibiotic sulfonamides are not likely to cause anaphylaxis (inter-reactions due to antibody production).
- T-cell-mediated (type IV), reactions (eg maculopapular skin rash) are less understood. It is difficult to exclude this possibility based on current knowledge.
- Some clinicians will limit exposure to classes in cases of severe reactions (Stevens Johnson syndrome/TEN).
- A deeper understanding of allergic mechanisms suggests that cross-reactivity between non-antibiotic sulfonamides or antibiotic sulfonamides might not be possible.
-
Bariatric surgery
- Dehydration: Do not take diuretics during the first 24 hours after bariatric surgery. Electrolyte disturbances or dehydration could occur.
- If necessary, diuretics can be resumed if oral fluid intake goals have been met.
-
Diabetes:
- Hydrochlorothiazide is not recommended for patients with diabetes mellitus or prediabetes.
-
Hepatic impairment
- Hydrochlorothiazide should be used with caution in patients suffering from severe hepatic dysfunction.
- Avoid electrolyte imbalances and acid/base imbalances in progressive or severe liver disease. This could lead to hepatic emboli/coma.
-
Hypercalcemia:
- Patients with hypercalcemia may be advised to limit their use
- Thiazide diuretics may lower renal calcium excretion.
-
Hypercholesterolemia:
- Patients with high or moderate cholesterol should not use Hydrochlorothiazide.
-
Hypokalemia
- Hypokalemia patients should be treated with Hydrochlorothiazide.
-
Parathyroid disease
- Thiazide diuretics decrease calcium excretion.
- Long-term use of these drugs can cause pathologic changes in parathyroid glands, including hypophosphatemia and hypercalcemia.
- It is best to stop using them before testing for parathyroid function.
-
Renal impairment
- Patients with impaired renal function may experience cumulative effects, including azotemia.
- Hydrochlorothiazide should be stopped in severe renal disease. It may cause azotemia.
- Uremia is home to the active metabolites methyldopa.
-
Systemic lupus erythematosus (SLE):
- SLE activation or exacerbation can be caused by hydrochlorothiazide.
Methyldopa and hydrochlorothiazide: Drug Interaction
|
Ajmaline |
Sulfonamides may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. |
|
Alcohol (Ethyl) |
May enhance the orthostatic hypotensive effect of Thiazide and Thiazide-Like Diuretics. |
|
Alfuzosin |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. |
|
Allopurinol |
Thiazide and Thiazide-Like Diuretics may enhance the potential for allergic or hypersensitivity reactions to Allopurinol. Thiazide and Thiazide-Like Diuretics may increase the serum concentration of Allopurinol. Specifically, Thiazide Diuretics may increase the concentration of Oxypurinol, an active metabolite of Allopurinol. |
|
Aminolevulinic Acid (Topical) |
Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). |
|
Amphetamines |
May diminish the antihypertensive effect of Antihypertensive Agents. |
|
Angiotensin-Converting Enzyme Inhibitors |
Thiazide and Thiazide-Like Diuretics may enhance the hypotensive effect of Angiotensin-Converting Enzyme Inhibitors. Thiazide and Thiazide-Like Diuretics may enhance the nephrotoxic effect of Angiotensin-Converting Enzyme Inhibitors. |
|
Anticholinergic Agents |
May increase the serum concentration of Thiazide and Thiazide-Like Diuretics. |
|
Antidiabetic Agents |
Thiazide and Thiazide-Like Diuretics may diminish the therapeutic effect of Antidiabetic Agents. |
|
Antidiabetic Agents |
Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. |
|
Antipsychotic Agents (Second Generation [Atypical]) |
Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). |
|
Barbiturates |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. |
|
Benazepril |
HydroCHLOROthiazide may enhance the hypotensive effect of Benazepril. HydroCHLOROthiazide may enhance the nephrotoxic effect of Benazepril. Benazepril may decrease the serum concentration of HydroCHLOROthiazide. |
|
Benperidol |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. |
|
Beta2-Agonists |
May enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. |
|
Bradycardia-Causing Agents |
May enhance the bradycardic effect of other Bradycardia-Causing Agents. |
|
Brigatinib |
May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. |
|
Brimonidine (Topical) |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. |
|
Calcium Salts |
Thiazide and Thiazide-Like Diuretics may decrease the excretion of Calcium Salts. Continued concomitant use can also result in metabolic alkalosis. |
|
CarBAMazepine |
Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of CarBAMazepine. Specifically, there may be an increased risk for hyponatremia. |
|
Cardiac Glycosides |
Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of Cardiac Glycosides. Specifically, cardiac glycoside toxicity may be enhanced by the hypokalemic and hypomagnesemic effect of thiazide diuretics. |
|
COMT Inhibitors |
May decrease the metabolism of COMT Substrates. |
|
Corticosteroids (Orally Inhaled) |
May enhance the hypokalemic effect of Thiazide and ThiazideLike Diuretics. |
|
Corticosteroids (Systemic) |
May enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. |
|
Cyclophosphamide |
Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of Cyclophosphamide. Specifically, granulocytopenia may be enhanced. |
|
Dexketoprofen |
May enhance the adverse/toxic effect of Sulfonamides. |
|
Dexmethylphenidate |
May diminish the therapeutic effect of Antihypertensive Agents. |
|
Diacerein |
May enhance the therapeutic effect of Diuretics. Specifically, the risk for dehydration or hypokalemia may be increased. |
|
Diazoxide |
Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of Diazoxide. |
|
Diazoxide |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. |
|
Dichlorphenamide |
Thiazide and Thiazide-Like Diuretics may enhance the hypokalemic effect of Dichlorphenamide. |
|
DULoxetine |
Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. |
|
Herbs (Hypertensive Properties) |
May diminish the antihypertensive effect of Antihypertensive Agents. |
|
Herbs (Hypotensive Properties) |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. |
|
Hypotension-Associated Agents |
Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. |
|
Ipragliflozin |
May enhance the adverse/toxic effect of Thiazide and Thiazide-Like Diuretics. Specifically, the risk for intravascular volume depletion may be increased. |
|
Ivabradine |
Thiazide and Thiazide-Like Diuretics may enhance the arrhythmogenic effect of Ivabradine. |
|
Ivabradine |
Bradycardia-Causing Agents may enhance the bradycardic effect of Ivabradine. |
|
Lacosamide |
Bradycardia-Causing Agents may enhance the AV-blocking effect of Lacosamide. |
|
Levodopa-Containing Products |
Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. |
|
Licorice |
May enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. |
|
Lormetazepam |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. |
|
Methenamine |
Thiazide and Thiazide-Like Diuretics may diminish the therapeutic effect of Methenamine. |
|
Methylphenidate |
May diminish the antihypertensive effect of Antihypertensive Agents. |
|
Midodrine |
May enhance the bradycardic effect of Bradycardia-Causing Agents. |
|
Molsidomine |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. |
|
Multivitamins/Fluoride (with ADE) |
May enhance the hypercalcemic effect of Thiazide and Thiazide-Like Diuretics. |
|
Multivitamins/Minerals (with AE, No Iron) |
Thiazide and Thiazide-Like Diuretics may increase the serum concentration of Multivitamins/Minerals (with AE, No Iron). Specifically, thiazide diuretics may decrease the excretion of calcium, and continued concomitant use can also result in metabolic alkalosis. |
|
Naftopidil |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. |
|
Neuromuscular-Blocking Agents (Nondepolarizing) |
Thiazide and Thiazide-Like Diuretics may enhance the neuromuscular-blocking effect of Neuromuscular-Blocking Agents (Nondepolarizing). |
|
Nicergoline |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. |
|
Nicorandil |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. |
|
Nitroprusside |
Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. |
|
Nonsteroidal Anti-Inflammatory Agents |
Thiazide and Thiazide-Like Diuretics may enhance the nephrotoxic effect of Nonsteroidal Anti-Inflammatory Agents. Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Thiazide and Thiazide-Like Diuretics. |
|
Opioid Agonists |
May enhance the adverse/toxic effect of Diuretics. Opioid Agonists may diminish the therapeutic effect of Diuretics. |
|
Oxcarbazepine |
Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of OXcarbazepine. Specifically, there may be an increased risk for hyponatremia. |
|
Pentoxifylline |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. |
|
Pholcodine |
Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. |
|
Phosphodiesterase 5 Inhibitors |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. |
|
Porfimer |
Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. |
|
Prostacyclin Analogues |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. |
|
Quinagolide |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. |
|
Reboxetine |
May enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. |
|
Ruxolitinib |
May enhance the bradycardic effect of Bradycardia-Causing Agents. Management: Ruxolitinib Canadian product labeling recommends avoiding use with bradycardia-causing agents to the extent possible. |
|
Selective Serotonin Reuptake Inhibitors |
May enhance the hyponatremic effect of Thiazide and Thiazide-Like Diuretics. |
|
Serotonin/Norepinephrine Reuptake Inhibitors |
May diminish the antihypertensive effect of Alpha2-Agonists. |
|
Terlipressin |
May enhance the bradycardic effect of Bradycardia-Causing Agents. |
|
Tofacitinib |
May enhance the bradycardic effect of Bradycardia-Causing Agents. |
|
Toremifene |
Thiazide and Thiazide-Like Diuretics may enhance the hypercalcemic effect of Toremifene. |
|
Valsartan |
HydroCHLOROthiazide may enhance the hypotensive effect of Valsartan. Valsartan may increase the serum concentration of HydroCHLOROthiazide. |
|
Verteporfin |
Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. |
|
Vitamin D Analogs |
Thiazide and Thiazide-Like Diuretics may enhance the hypercalcemic effect of Vitamin D Analogs. |
|
Yohimbine |
May diminish the antihypertensive effect of Antihypertensive Agents. |
|
Risk Factor D (Consider therapy modification) |
|
|
Amifostine |
Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. |
|
Beta-Blockers |
|
|
Bile Acid Sequestrants |
May decrease the absorption of Thiazide and Thiazide-Like Diuretics. The diuretic response is likewise decreased. |
|
Ceritinib |
Bradycardia-Causing Agents may enhance the bradycardic effect of Ceritinib. Management: If this combination cannot be avoided, monitor patients for evidence of symptomatic bradycardia, and closely monitor blood pressure and heart rate during therapy. Exceptions are discussed in separate monographs. |
|
Iron Preparations |
May decrease the serum concentration of Methyldopa. Exceptions: Ferric Carboxymaltose; Ferric Gluconate; Ferric Hydroxide Polymaltose Complex; Ferric Pyrophosphate Citrate; Ferumoxytol; Iron Dextran Complex; Iron Isomaltoside; Iron Sucrose. |
|
Lithium |
Thiazide and Thiazide-Like Diuretics may decrease the excretion of Lithium. |
|
Mirtazapine |
May diminish the antihypertensive effect of Alpha2-Agonists. Management: Consider avoiding concurrent use. If the combination cannot be avoided, monitor for decreased effects of alpha2-agonists if mirtazapine is initiated/dose increased, or increased effects if mirtazapine is discontinued/dose decreased. |
|
Multivitamins/Minerals (with ADEK, Folate, Iron) |
May decrease the serum concentration of Methyldopa. Management: Consider separating doses of these products by 2 or more hours to minimize this interaction; however, the success of this action appears limited. Monitor for decreased therapeutic effects of methyldopa with concurrent use. |
|
Obinutuzumab |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. |
|
Riluzole |
Methyldopa may enhance the adverse/toxic effect of Riluzole. Specifically, the risk of hepatotoxicity may be increased. Management: Consider alternatives to methyldopa in patients receiving treatment with riluzole due to the potential for additive hepatotoxicity. |
|
Siponimod |
Bradycardia-Causing Agents may enhance the bradycardic effect of Siponimod. Management: Avoid coadministration of siponimod with drugs that may cause bradycardia. |
|
Sodium Phosphates |
Diuretics may enhance the nephrotoxic effect of Sodium Phosphates. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with diuretics, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, hydrate adequately and monitor fluid and renal status. |
|
Topiramate |
Thiazide and Thiazide-Like Diuretics may enhance the hypokalemic effect of Topiramate. Thiazide and Thiazide-Like Diuretics may increase the serum concentration of Topiramate. Management: Monitor for increased topiramate levels/adverse effects (e.g., hypokalemia) with initiation/dose increase of a thiazide diuretic. Closely monitor serum potassium concentrations with concomitant therapy. Topiramate dose reductions may be necessary. |
|
Tricyclic Antidepressants |
May diminish the antihypertensive effect of Alpha2-Agonists. Management: Consider avoiding this combination. If used, monitor for decreased effects of the alpha2-agonist. Exercise great caution if discontinuing an alpha2-agonist in a patient receiving a TCA. |
|
Risk Factor X (Avoid combination) |
|
|
Aminolevulinic Acid (Systemic) |
Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). |
|
Bromperidol |
Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. |
|
Dofetilide |
HydroCHLOROthiazide may enhance the QTc-prolonging effect of Dofetilide. HydroCHLOROthiazide may increase the serum concentration of Dofetilide. |
|
Fexinidazole [INT] |
Thiazide and Thiazide-Like Diuretics may enhance the arrhythmogenic effect of Fexinidazole [INT]. |
|
Fexinidazole [INT] |
Bradycardia-Causing Agents may enhance the arrhythmogenic effect of Fexinidazole [INT]. |
|
Iobenguane Radiopharmaceutical Products |
Methyldopa may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer methyldopa until at least 7 days after each iobenguane dose. |
|
Levosulpiride |
Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of Levosulpiride. |
|
Mecamylamine |
Sulfonamides may enhance the adverse/toxic effect of Mecamylamine. |
|
Monoamine Oxidase Inhibitors |
May enhance the adverse/toxic effect of Methyldopa. |
|
Promazine |
Thiazide and Thiazide-Like Diuretics may enhance the QTc-prolonging effect of Promazine. |
Monitoring parameters:
- Blood pressure;
- CBC;
- liver enzymes (periodically during the first 6 to 12 weeks or when unexplained fever occurs);
- Serum electrolytes, BUN, creatinine;
- Coombs test (direct) (may obtain prior to initiation and at 6 and 12 months).
How to administer Methyldopa and hydrochlorothiazide (Hydromet)?
When the dose of methyldopa component is higher, consider administration in the evening to minimize daytime sedation.
Mechanism of action of Methyldopa and hydrochlorothiazide (Hydromet):
- Methyldopa stimulates the central alpha-adrenergic receptors through a false transmitter, which results in decreased sympathetic outflow to kidneys, heart and peripheral vasculature.
- Hydrochlorothiazide reduces sodium reabsorption from the distal tubules, causing an increase in excretion of sodium, water, as well as potassium ions.
International Brand Names of Methyldopa and hydrochlorothiazide:
- Apo-Methazide
- Dopatens-H
- Hydromet
- Tensifort
Methyldopa and hydrochlorothiazide Brand Names in Pakistan:
There is no brand available in Pakistan.
.png)


