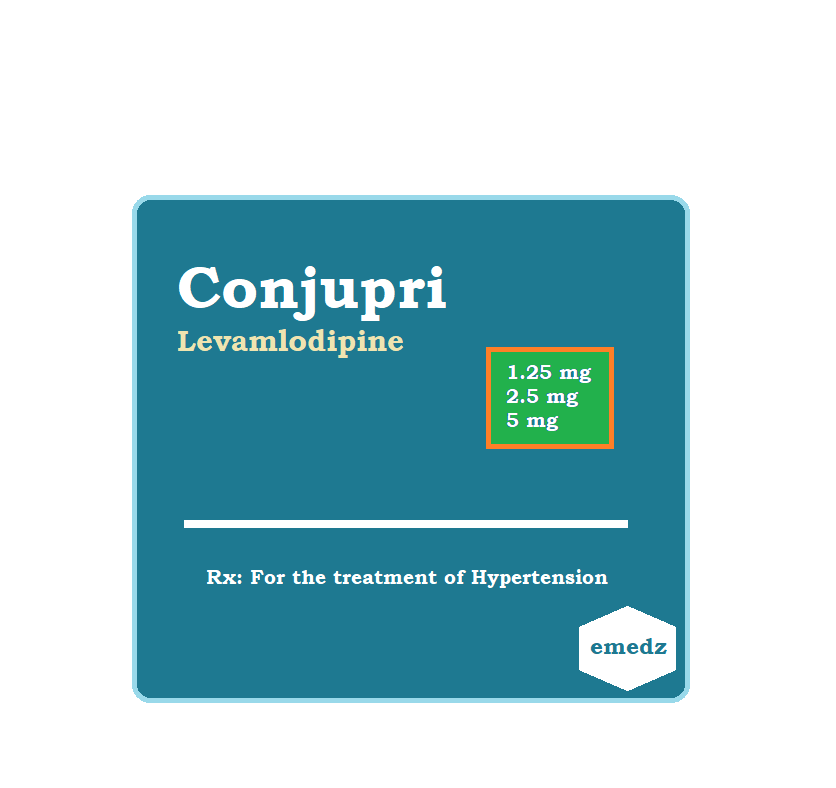
Levamlodipine (Conjupri) is the active isomer of amlodipine. It is used orally for the treatment of patients with hypertension.
Levamlodipine Uses:
- Hypertension:
- Adults and kids aged six and older who have hypertension are administered it to treat it.
Levamlodipine Dose in Adults:
Hypertension:
- Note: When treating individuals whose blood pressure is at least 20/10 mm Hg above target, it may first be combined with another suitable medication, such as an angiotensin-converting enzyme inhibitor, angiotensin II receptor blocker, or a thiazide diuretic.
- Some doctors advise an initial trial of monotherapy for individuals whose blood pressure is less than 20/10 mm Hg over the target, yet eventually, patients will need combo medication.
- Orally: initially 1.25 to 2.5 mg once daily.
- As per patients' response and need, titrate every one to two weeks.
- The maximum daily dosage is 5 mg.
- With larger dosages, the antihypertensive impact is lessened and there is a greater possibility of side effects.
Levamlodipine dose in children:
-
Hypertension:
- For young children and teenagers aged 6 to 17:
- 1.25 to 2.5 mg orally, once a day.
Levamlodipine Pregnancy Risk Category: N
- Levamlodipine and Dextro amlodipine can be thought of as the racemic components of amlodipine.
- There is no placental barrier to amlodipine.
- For additional information, Refer to the amlodipine monograph.
Use during breastfeeding:
- Breast milk contains amlodipine.
- Amlodipine can be described as a racemic combination of levamlodipine, the pharmacologically active Iomer, and dextro amlodipine.
- For more information, refer to the amlodipine monograph
Dose in kidney disease:
- No dosage adjustments are necessary in kidney impairment in children and adolescents from 6 to 17 years.
Levamlodipine Dose in liver disease:
- Hypertension:
- 1.25 mg once each day at first.
- In individuals with severe hepatic impairment, titrate gradually.
Common Side Effects of Levamlodipine:
- Cardiovascular:
- Edema
Less Common Side Effects of Levamlodipine:
- Cardiovascular:
- Palpitations
- Flushing
- Central nervous system:
- Fatigue
- Dizziness
- Drowsiness
- Gastrointestinal:
- Nausea
- Abdominal pain
Contraindications to Levamlodipine:
- responses due to allergies to levamlodipine, amlodipine, or any other formulation ingredient.
Warnings and precautions
- Angina and myocardial Infarction
- In case of reports, angina or myocardial enlargement were more common after treatment initiation or dosage adjustment of dihydropyridine calciumchannel blockers.
- Patients with obstructive cardiomyopathy may experience tachycardia, especially if there is no concurrent beta-blockade.
- Hypotension
- Some individuals' symptoms of hypotension may be present.
- Hypotension is unlikely because of the slow development.
- The rate of BP reduction should be proportionate to the clinical circumstances of the patient.
- Peripheral edema
- The most frequent adverse effect is peripheral edoema. Peripheral edoema may appear 2 to 3 weeks after commencing medication.
- Aortic stenosis
- Patients suffering from severe aortic stenosis must be cautious.
- It can cause hypotension and reduce coronary perfusion. This could lead to ischemia.
- Heart failure:
- Calcium channel blockers are to be kept away from by patients with lower ejection fractions whenever possible.
- Hepatic impairment
- Patients with hepatic impairment should be cautious.
- Patients may need lower starting doses.
- Patients with significant hepatic impairment ought to be able to gradually increase their dosage.
- Hypertrophic cardiomyopathy and outflow tract obstruction
- The signs of this illness might get worse if the afterload is reduced.
- When using amlodipine, patients with hypertrophic cardiomyopathy or outflow tract blockage should exercise caution.
Levamlodipine: Drug Interaction
Risk Factor C (Monitor therapy) |
|
|
Alfuzosin |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Alpha1-Blockers |
The hypotensive effects of calcium channel blockers may be strengthened. |
|
Amphetamines |
may lessen the effectiveness of antihypertensive agents. |
|
Antipsychotic Agents (Second Generation [Atypical]) |
Antipsychotic drugs' hypotensive effects may be enhanced by blood pressure-lowering medications (Second Generation [Atypical]). |
|
ARIPiprazole |
ARIPiprazole's serum levels may rise in response to CYP3A4 Inhibitors (Weak). Management: Keep an eye out for enhanced pharmacologic effects of aripiprazole. Depending on the concurrent therapy and/or the indication, aripiprazole dosage modifications may or may not be necessary. For detailed advice, refer to the whole interaction monograph. |
|
Atosiban |
Calcium channel blockers may intensify Atosiban's harmful or hazardous effects. Particularly, pulmonary edoema and/or dyspnea may be at higher risk. |
|
Barbiturates |
Calcium Channel Blockers' metabolic rate could be increased. Management: Keep an eye out for any diminished therapeutic benefits of barbiturate medication when concurrently using calcium channel blockers. There may need to be dosage modifications with calcium channel blockers. The concurrent use of phenobarbital and nimodipine is not recommended. |
|
Barbiturates |
Blood pressure-lowering drugs could intensify their hypotensive effects. |
|
Benperidol |
Blood pressure-lowering drugs could intensify their hypotensive effects. |
|
Bosentan |
may reduce the serum concentration of CYP3A4 substrates (High risk with Inducers). |
|
Brigatinib |
Antihypertensive medications' potency can be decreased. Brigatinib may enhance the bradycardic activity of antihypertensive agents. |
|
Brimonidine (Topical) |
Blood pressure-lowering drugs could intensify their hypotensive effects. |
|
Calcium Channel Blockers (Nondihydropyridine) |
Calcium channel blockers' hypotensive effects may be exacerbated by the calcium channel blocker dihydropyridine (Nondihydropyridine). Nondihydropyridine, a calcium channel blocker, may result in a rise in serum calcium channel blocker concentration (Dihydropyridine). |
|
Calcium Salts |
may lessen the therapeutic effects of calcium channel blockers. |
|
Clopidogrel |
Calcium channel blockers may decrease the therapeutic effectiveness of clopidogrel. |
|
CycloSPORINE (Systemic) |
When calcium channel blockers (Dihydropyridine) are administered, the serum levels of cycloSPORINE may increase (Systemic). When using CycloSPORINE (Systemic), blood levels of calcium channel blockers may increase (Dihydropyridine). |
|
CYP3A4 Inducers (Moderate) |
may lower the serum level of CYP3A4 substrates (High risk with Inducers). |
|
CYP3A4 Inhibitors (Moderate) |
Levamlodipine serum levels can rise. |
|
CYP3A4 Inhibitors (Strong) |
Levamlodipine serum levels can rise. |
|
Dapoxetine |
may intensify calcium channel blockers' orthostatic hypotensive effects. |
|
Deferasirox |
may reduce the concentration of CYP3A4 substrates in serum (High risk with Inducers). |
|
Dexmethylphenidate |
can lessen an antihypertensive drug's therapeutic impact. |
|
Diazoxide |
Blood pressure-lowering medicines may strengthen their hypotensive effects. |
|
Dofetilide |
Dofetilide's serum levels may rise in the presence of CYP3A4 Inhibitors (Weak). |
|
DULoxetine |
The hypotensive impact of DULoxetine may be enhanced by blood pressure lowering medications. |
|
Efavirenz |
Calcium Channel Blockers' serum concentration can drop. |
|
Erdafitinib |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). |
|
Flibanserin |
The serum levels of Flibanserin may rise in response to CYP3A4 Inhibitors (Weak). |
|
Fluconazole |
Calcium Channel Blockers' serum levels can rise. |
|
Herbs (Hypotensive Properties) |
Blood pressure-lowering drugs could intensify their hypotensive effects. |
|
Hypotension-Associated Agents |
Blood pressure lowering drugs have the potential to enhance the hypotensive impact of hypotension-associated agents. |
|
Ivosidenib |
may reduce the serum concentration of CYP3A4 substrates (High risk with Inducers). |
|
Levodopa-Containing Products |
Medications that reduce blood pressure may increase the hypotensive effects of levodopa-containing products. |
|
Lormetazepam |
Blood pressure-lowering drugs could intensify their hypotensive effects. |
|
Lovastatin |
The serum levels of Lovastatin may rise when taken with Levamlodipine. |
|
Magnesium Salts |
Calcium channel blockers could make magnesium salts more harmful or poisonous. Calcium Channel Blockers' hypotensive effects may be strengthened by magnesium salts. |
|
Melatonin |
may reduce the effectiveness of calcium channel blockers as an antihypertensive (Dihydropyridine). |
|
Methylphenidate |
May lessen the effectiveness of antihypertensive agents. |
|
Molsidomine |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Naftopidil |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Neuromuscular-Blocking Agents (Nondepolarizing) |
The neuromuscular-blocking impact of neuromuscular-blocking agents may be enhanced by calcium channel blockers (Nondepolarizing). |
|
Nicergoline |
Blood pressure-lowering drugs could intensify their hypotensive effects. |
|
Nicorandil |
Blood pressure-lowering drugs could intensify their hypotensive effects. |
|
NiMODipine |
NiMODipine's serum levels may rise in the presence of CYP3A4 Inhibitors (Weak). |
|
Nitroprusside |
Nitroprusside's hypotensive impact may be strengthened by blood pressure-lowering medications. |
|
Pentoxifylline |
Blood pressure-lowering medicines may strengthen their hypotensive effects. |
|
Pholcodine |
Pholcodine's hypotensive impact may be strengthened by blood pressure lowering medications. |
|
Phosphodiesterase 5 Inhibitors |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Prostacyclin Analogues |
Blood pressure-lowering medicines may strengthen their hypotensive effects. |
|
Quinagolide |
Blood pressure-lowering medicines may strengthen their hypotensive effects |
|
QuiNIDine |
Calcium channel blockers may reduce the level of quiNIDine in the blood (Dihydropyridine). Calcium channel blockers may cause an increase in the blood levels of quinidine (Dihydropyridine). In response to quinine, blood levels of calcium channel blockers may increase (Dihydropyridine). |
|
Sarilumab |
may reduce the concentration of CYP3A4 substrates in serum (High risk with Inducers) |
|
Siltuximab |
could reduce the serum concentration of CYP3A4 substrates (High risk with Inducers). |
|
Tacrolimus (Systemic) |
Tacrolimus serum levels may rise when Calcium Channel Blockers (Dihydropyridine) are used (Systemic). |
|
Tocilizumab |
Could reduce the serum concentration of CYP3A4 substrates (High risk with Inducers). |
|
Yohimbine |
may make antihypertensive medications less effective. |
|
Risk Factor D (Consider therapy modification) |
|
|
Amifostine |
Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. |
|
Antifungal Agents (Azole Derivatives, Systemic) |
Calcium Channel Blockers' harmful or toxic effects might be exacerbated. In particular, itraconazole may make verapamil or diltiazem's unfavourable inotropic effects worse. Calcium Channel Blockers' metabolism may be slowed down by antifungal agents (systemic azole derivatives). Fluconazole and isavuconazonium, which are covered in different monographs, probably have less powerful effects than those of other azoles. Treatment: Itraconazole should not be used concurrently with felodipine or nisoldipine. With any such combination, regular monitoring is advised; calcium channel blocker dose decreases could be necessary. Fluconazole and isavuconazonium sulphate are exceptions. |
|
CarBAMazepine |
Calcium Channel Blockers' metabolism might be accelerated (Dihydropyridine). In individuals taking concurrent carbamazepine, consider adjusting the dosage of calcium channel blockers (CCBs) or switching to an alternative form of treatment. The Canadian labelling for nimodipine expressly forbids using it alongside carbamazepine. |
|
Cimetidine |
Calcium Channel Blockers' serum levels can rise. Management: Take cimetidine substitutes into consideration. If there is no acceptable substitute, watch for increased calcium channel blocker effects after starting or increasing the dosage of cimetidine and decreased effects after stopping or decreasing the dosage. |
|
CYP3A4 Inducers (Strong) |
may speed up CYP3A4 substrate metabolism (High risk with Inducers). Management: Take into account a substitute for one of the interfering medications. Specific contraindications may apply to some combinations. the relevant manufacturer's label. |
|
Dabrafenib |
may lower the serum level of CYP3A4 substrates (High risk with Inducers). Management: When feasible, look for substitutes for the CYP3A4 substrate. If concurrent therapy cannot be avoided, pay special attention to the substrate's clinical consequences (particularly therapeutic effects). |
|
Enzalutamide |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). Treatment: Enzalutamide should not be used concurrently with CYP3A4 substrates that have a limited therapeutic index. Enzalutamide use, like with the use of any other CYP3A4 substrate, should be done cautiously and under close observation. |
|
Fosphenytoin |
Calcium channel blockers may raise the level of fosphenytoin in the blood. Monitoring for phenytoin toxicity while using a calcium channel blocker (CCB) at the same time or reduced phenytoin effects while stopping the CCB are the two management options. Check for diminished therapeutic effects of CCB. The Canadian labelling for nimodipine specifically forbids the use of phenytoin. |
|
Lemborexant |
Lemborexant's serum levels may rise in the presence of CYP3A4 Inhibitors (Weak). Management: When used in conjunction with weak CYP3A4 inhibitors, a maximum daily dose of 5 mg of lemborexant is advised. |
|
Lomitapide |
The blood levels of lomitapide may rise in the presence of CYP3A4 Inhibitors (Weak). Treatment: Patients taking 5 mg/day of lomitapide may continue doing so. Patients using 10 mg or more of lomitapide per day should cut their dosage in half. Maximum adult dosage of 30 mg/day may then be reached by titrating the lomitapide dose. |
|
Lorlatinib |
may lower the serum level of CYP3A4 substrates (High risk with Inducers). Management: Avoid using lorlatinib at the same time as any CYP3A4 substrates for which even a small drop in blood levels of the substrate might result in therapeutic failure and negative clinical outcomes. |
|
Macrolide Antibiotics |
Calcium Channel Blockers' metabolic rate could be decreased. Use a noninteracting macrolide as a possible management strategy. The Canadian labelling for felodipine expressly advises against using it in conjunction with clarithromycin. Azithromycin (Systemic), Fidaxomicin, Roxithromycin, and Spiramycin are exceptions. |
|
Mitotane |
May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. |
|
Obinutuzumab |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. |
|
Phenytoin |
The blood levels of phenytoin may rise when calcium channel blockers are used. Calcium Channel Blockers' serum levels may be reduced by phenytoin. Avoid combining nimodipine or nifedipine with phenytoin for management. With any concurrent usage, keep an eye out for phenytoin toxicity and/or diminished calcium channel blocker effects. |
|
Rifamycin Derivatives |
Calcium Channel Blockers' serum concentration can drop. This predominantly affects calcium channel blockers used orally. Management: Using rifampin with certain calcium channel blockers is not advised according to the labelling in the US and Canada. Look up the relevant labels. |
|
Simvastatin |
Simvastatin's serum levels might rise as a result of levamlodipine. Management: When at all feasible, refrain from taking simvastatin and amlodipine together. If combined, stay away from simvastatin dosages higher than 20 mg per day (for adults). |
|
Sincalide |
The therapeutic benefit of Sincalide may be reduced by medications that affect gallbladder function. Prior to using sincalide to induce gallbladder contraction, you should think about stopping any medications that can impair gallbladder motility. |
|
Triazolam |
Triazolam's serum levels may rise in the presence of CYP3A4 Inhibitors (Weak). Management: If a patient is using a concurrent mild CYP3A4 inhibitor, consider reducing the dosage of triazolam. |
|
Ubrogepant |
It's possible that CYP3A4 Inhibitors (Weak) will raise the level of ubrogepant in the blood. Treatment: The initial and second doses of ubrogepant in patients using mild CYP3A4 inhibitors should be no more than 50 mg each. |
|
Risk Factor X (Avoid combination) |
|
|
Bromperidol |
The hypotensive impact of bromperidol may be enhanced by blood pressure lowering medications. Blood Pressure Lowering Agents' hypotensive effects may be lessened by bromperidol. |
|
Pimozide |
Pimozide's serum levels may rise in response to CYP3A4 Inhibitors (Weak). |
Monitoring parameters:
Monitor the heart rate and Blood pressure.
High blood pressure in adults: The 2017 Guideline for the Prevention, Detection, Evaluation, and Management.
- A 10-year atherosclerotic cardiovascular disease risk of 10% or confirmed hypertension plus a history of cardiovascular disease:
- Recommended target blood pressure is 130/80 mm Hg.
- A confirmed case of hypertension without signs of an elevated risk of atherosclerotic cardiovascular disease:
- Recommended target blood pressure is 130/80 mm Hg.
Diabetes and hypertension: The American Diabetes Association guidelines.
- Patients between the ages of 18 and 65 who have a 10-year atherosclerotic cardiovascular disease risk of less than 15% and do not have the atherosclerotic cardiovascular disease:
- It is advised to maintain a target blood pressure of 140/90 mm Hg.
- Patients between the ages of 18 and 65 with known atherosclerotic cardiovascular disease or a 10% risk in the next ten years:
- If it is possible to do so safely, a target blood pressure of 130/80 mm Hg may be recommended.
- Patients >65 years old (in good, complicated, or mediocre health):
- It is advised to maintain a target blood pressure of 140/90 mm Hg.
- Patients >65 years of age (very complex/poor health):
- It is advised to maintain a target blood pressure of 150/90 mm Hg.
How to administer Levamlodipine?
- It may be taken once daily without regard to meals.
Mechanism of action of Levamlodipine:
- It immediately affects the blood vessel and smooth muscles, decreasing blood pressure and reducing peripheral vascular resistance.
- Amlodipine, a dihydropyridine calcium-channel blocker, acts by blocking transmembrane calcium influx into calcium ions.
- It is most effective in the smooth muscle cells of the vessels but less so in the cardiac muscle cells.
- The pharmacologically potent antihypertensive isomer of levamlodipine, amlodipine, is a 1:1 racemic combination of levamlodipine and dextro-amlodipine.
- Protein binding:
- ~93%.
- Onset:
- Gradual.
- Duration:
- less than or more than 24 hours.
- Excretion:
- Urine (10% of total dose as unchanged drug, 60% of total dose as metabolites).
- Metabolism:
- Hepatic (~90%) to inactive metabolites.
- Half-life elimination:
- Terminal (biphasic): ~30 to 50 hours;
- increased with hepatic dysfunction.
- Bioavailability:
- 64% to 90%.
- Time to peak:
- 6 to 12 hours.
- Clearance:
- Clearance of the drug may be decreased in patients with hepatic insufficiency or moderate to severe heart failure;
- Wweight-adjusted clearance in children >6 years of age is similar to adults
Levamlodipine Brand Names (International):
- S-Ambes
- Conjupri
Levamlodipine Brand Names in Pakistan:
No Brands Available in Pakistan.
.png)


